Cashless
The redesigned IPD cashless claims workflow, powered by the HCX protocol, provides a valuable insight into the seamless and efficient processing of claim requests. HCX brings interoperability and transparency in the claim adjudication process, ensuring that claims are handled promptly and effectively.
Ref: Typical IPD cashless claims workflow
Important note : The work stream's original diagram representing the overall workflow of the reimagined IPD cashless using HCX is available here. Based on initial feedback for improving the readability, the sections below detail it in multiple diagrams representing each stage separately.
IPD cashless claims through HCX
Coverage eligibility flow
The coverage eligibility check for the beneficiary is usually the first stage in an IPD service delivery and claims process. HCX facilitates a structured and timely response to the coverage eligibility check request and response delivery for stakeholders. The following diagram describes the steps and stakeholders involved in the coverage eligibility flow.

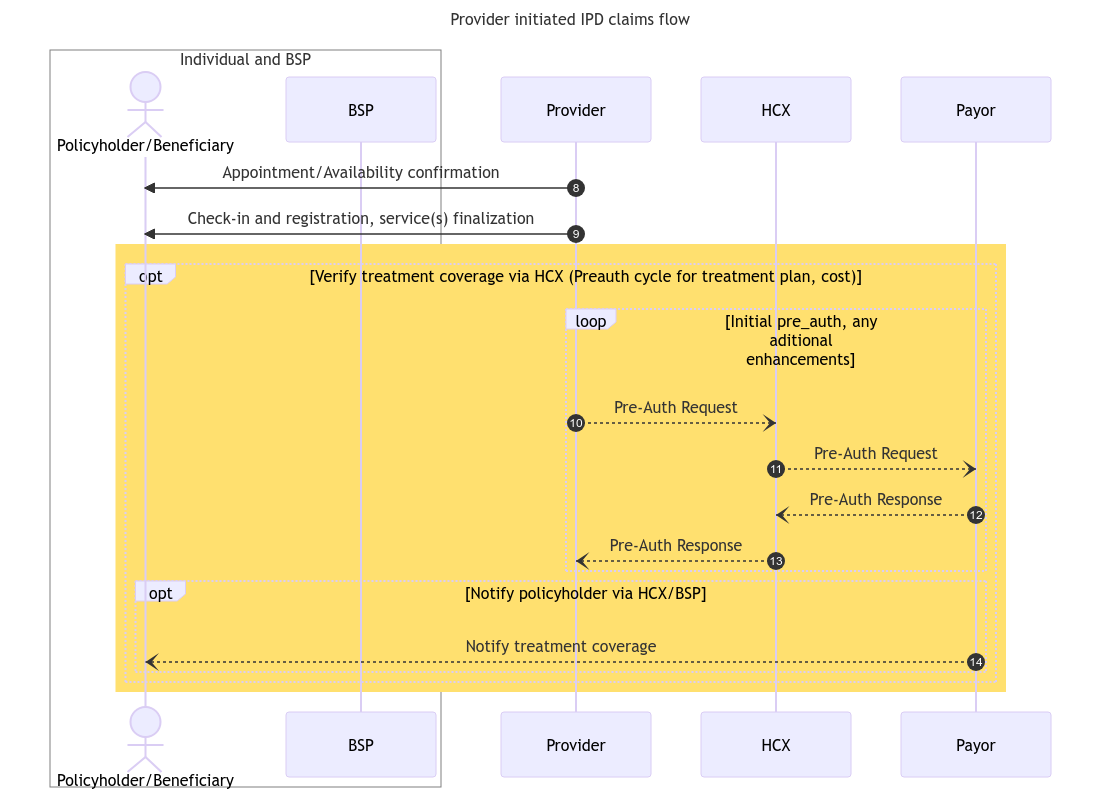
Pre-auth flow
After the coverage eligibility process, the provider determines the required services or treatment plan for the beneficiary's requirements, along with the associated expenses, and submits it to the payer for pre-authorization. The following diagram provides an overview of the steps and stakeholders involved in the pre-auth flow.
Claims flow
Once the Provider has provided the services to the beneficiary in accordance with the treatment plan, it initiates the claim request with the concerned payer through HCX, furnishing the necessary information for the claim adjudication. The following diagram describes the steps and stakeholders involved in the claims flow through HCX.
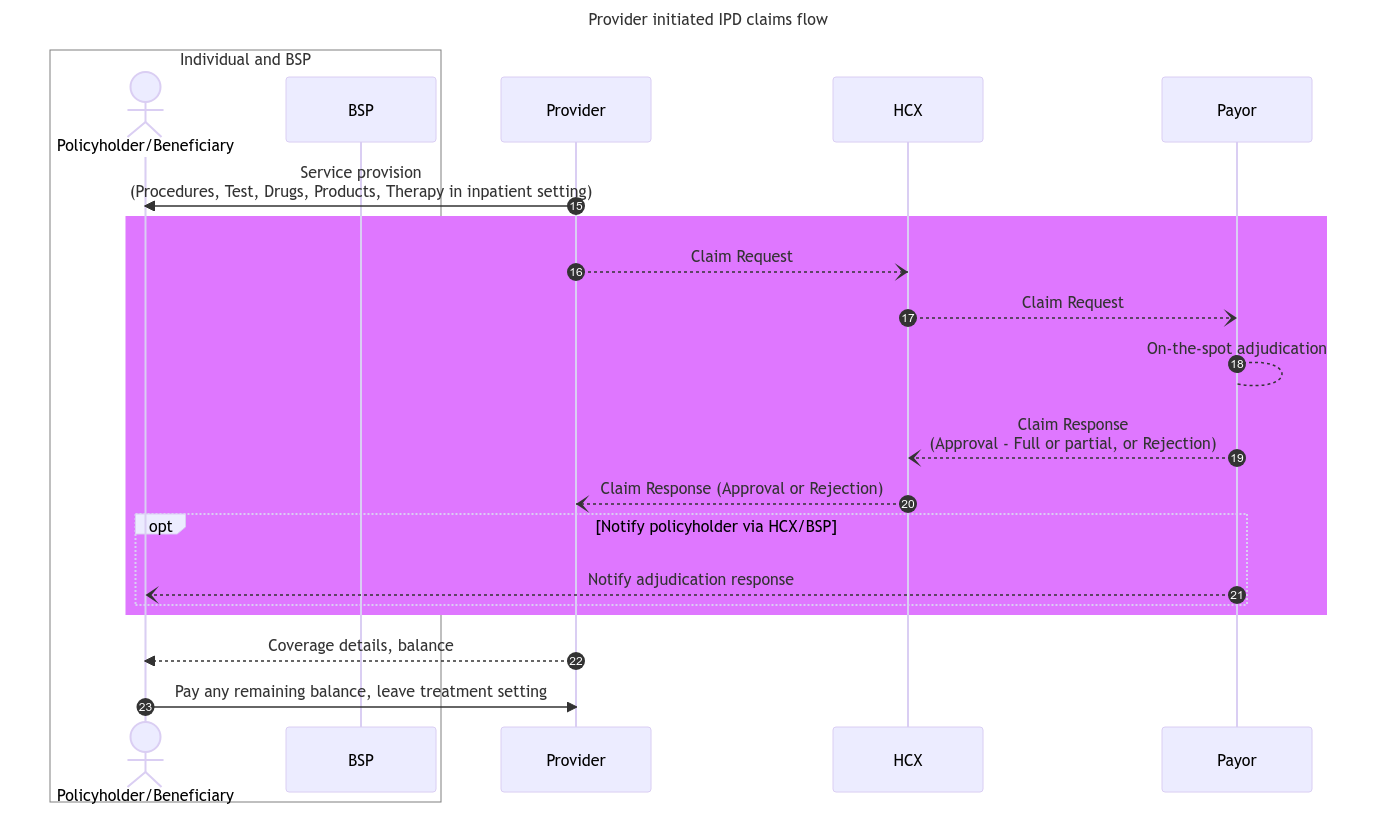
The next section describes IPD reimbursement claims workflow leveraging HCX protocol.
Last updated
Was this helpful?